
RAISING AWARENESS THROUGH EDUCATION
PROMOTING PREVENTION & EARLY DETECTION CAMPAIGNING FOR CHANGE
SKCIN: THE KAREN CLIFFORD SKIN CANCER CHARITY / REGISTERED CHARITY: 1150048

WE NEED YOUR HELP! PLEASE HELP US TO STOP SKIN CANCER TAKING MORE LIVES. WE ARE HUGELY GRATEFUL FOR YOUR SUPPORT.
Melanoma Skin Cancer
about each type of skin cancer and what signs of change you should look out for - EARLY DETECTION IS VERY IMPORTANT!


Melanoma
Melanoma is the least common but most dangerous type of skin cancer. It is often fast growing and can spread to other parts of the body to form a new cancer.
- Melanoma is the most dangerous form of skin cancer.
- Melanomas often look like moles and some originate from moles.
- Most cases are caused by over-exposure to the sun and/or sunbeds.
- Intense and occasional UV exposure and sunburn from the sun and/or sunbeds is a major cause.
- Melanoma develops when unrepaired DNA damage to skin cells triggers mutations that cause the cells to rapidly multiply and form malignant tumours.
- Melanoma tumours originate in the pigment producing melanocytes located in the basal layer of the skin's epidermis.
- If melanoma is not detected and treated at an early stage it can spread to other parts of the body, is difficult to treat and can be fatal.
- It is not the most common of skin cancer but causes the most deaths.
- In 2010 there were 12,818 new cases of melanoma in the UK.
- 7 people die every day from melanoma in the UK.
- Melanoma is now one of the biggest cancer killers in 15-34 year olds.
- An estimated 8,790 people die annually from melanoma in the US.
There are 4 basic types of melanoma:
- Superficial Spreading Melanoma (the most common)
- Lentigo Maligna
- Arcal Lentiginous Melanoma
- Nodular Melanoma
Superficial Spreading Melanoma.
This is the most common type of melanoma.
This type of melanoma begins 'in situ' which means that it occupies the top layers of the skin for a fairly long time before penetrating more deeply.
This type of melanoma is most often seen in younger people.
Superficial Spreading Melanoma can occur in a previously benign mole and can be found almost anywhere on the body, although the most common sites are: legs in women, trunk in men and upper back on both.
For example images and what to look out for go to Examples, signs and symptoms >
Lentigo Maligna
This type of melanoma is similar to Superficial Spreading Melanoma.
This type of melanoma begins 'in situ' which means that it occupies the top layers of the skin for a fairly long time before penetrating more deeply.
Lentigo Melanoma is most commonly found in the elderly, on chronically sun damaged skin, on areas such as face, ears, arms and upper body.
For example images and what to look out for go to Examples, signs and symptoms >
Arcal Lentiginous Melanoma
Again, this type of melanoma begins 'in situ' which means that it occupies the top layers of the skin for a fairly long time before penetrating more deeply.
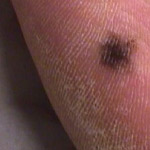
However, unlike other melanomas it is usually located on the palms of hands, soles of feet and under nails and appears as a black discolouration.
This type of melanoma is more common in Asians and African-Americans and less common among Caucasians and can advance faster than Lentigo Maligna and Superficial Spreading Melanoma.
For example images and what to look out for go to Examples, signs and symptoms >
Nodular Melanoma
This type of melanoma is the most aggressive form, found in around 10-15% of cases.
The tumour is recognized when it becomes a bump (which can vary in colour) and is usually invasive by the time of diagnosis.
The most common sites for Nodular Melanoma are the arms, legs and trunk and scalp in men, but can appear in other areas of the body.
For example images and what to look out for go to Examples, signs and symptoms >
Checking your skin thoroughly for any signs of change at least once a month, is very important for the early detection of any skin cancer.
However, when it comes to melanoma, which can be fatal if not detected early enough it is absolutely vital that you know your skin, know what signs to look for and seek professional medical advice with ANYTHING you feel uncertain of or are worried about!
If you go to your GP, to be told that your concern is nothing to worry about, but your are still unsure and worried, it is important to request a referral for expert advice from a trained skin specialist. GP's who are not trained sufficiently can and do miss melanomas - so make sure you seek professional advice and/or have a full screening to eliminate any risks and uncertainty.
To help you remember and recognise the major warning signs of melanoma, the most commonly used strategy is: 'The ABCDE of Melanoma' (although the same strategy should be used for the detection of Nodular Melanoma). Use the information below to help you know what to look for when checking your skin - However, it is important to acknowledge that all melanomas can differ considerably in size, shape and colour, so the images used here are to be used as a guideline only. It is also important to acknowledge that these are close-up images and that if located early enough they can appear very small on the body. It is therefore a good idea to use a magnifying glass to help you check smaller potential abnormalities.
Information on how to check your skin properly can be found here > How to check your skin -
but essentially you need to make sure you check EVERYWHERE and get someone to help check hard to see places.
The ABCDE of Melanoma:
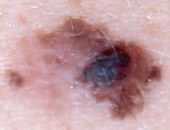
When one half of the mole does not match the other half
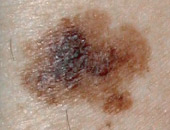
When the borders of the mole are irregular, ragged or blurred
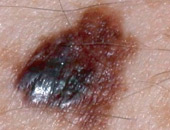
When the colour of the mole varies throughout / no uniform pigmentation

When the diameter is greater than 6mm (but it could be smaller)

Changes in the mole over variable time - weeks, months or years

WARNING
Nodular Melanomas do not typically follow these guidelines - see below for guidance
You should consult your doctor if you develop any of the following signs:
- Changing shape, particularly getting an irregular outline.
- Changing colour/getting darker, becoming patchy or multi-shaded.
- An existing mole getting bigger or a new mole growing quickly.
- A mole starts to itch, becomes painful, starts bleeding, becomes crusty or inflamed.
How to detect Nodular Melanoma:
Nodular melanomas do not follow the ABCDE of Melanoma outlined above.
They are more even in colour and have even edges.
They grow fast, downward and become quickly invasive (within months!).
A good way to remember what to look out for is EFG:
E = ELEVATED, F = FIRM TO TOUCH, G = GROWING
Nodular melanomas are usually black, but occasionally are blue, grey, white, brown, tan, red or skin tone. The images below show some examples, but if you detect any lump on the skin that is growing quickly - seek professional medical advice immediately.




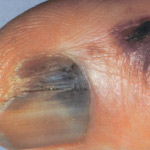
Examples of Arcal Lentiginous Melanoma
Unlike other melanomas Arcal Lentiginous Melanoma is usually located on the palms of hands, soles of feet and under nails and appears as a black discolouration.
This type of melanoma is more common in Asians and African-Americans and less common among Caucasians and can advance faster than Lentigo Maligna and Superficial Spreading Melanoma.
These are examples of Arcal Lentiginous Melanoma:


Everyone is at some risk of developing melanoma, but your level of risk is dependent on several factors - these include: History of sun exposure, skin type, moles, personal history of melanoma, family history of melanoma and weakened immune system. We look at each of these below in more detail:
Sun /UV Exposure:
Over exposure to UV radiation from the sun and/or sunbeds/booths is the main cause of melanoma.
Short, Intense and occasional UV exposure and history of sunburn from the sun and/or sunbeds is a major cause and considerably increases a person's risk of developing the disease.
Blistering sunburn in early childhood can significantly increase an individuals risk, but cumulative sun exposure is also considered a major cause. Using sunbeds for the first time before the age of 35 increases the risk of developing melanoma skin cancer by 59%. Regular sunbed use under the age of 30 increases the risk of skin cancer by an alarming 75%!
Skin Type:
As with all skin cancers, those with fairer skin who burn more easily are at greater risk of damaging their skin which can ultimately lead to skin cancer and melanoma. For further, in-depth information on skin types and associated risk click here >
Moles:
Almost everyone has moles, but generally speaking the more moles a person has, the greater risk of developing melanoma. There are 2 types of moles: normal moles and atypical moles - also known as dysplastic nevi. These can be a precursor to melanoma.
Personal History:
Anyone with a history of melanoma is at a greater risk of recurrence and those with a history of non melanoma skin cancer such as basal cell carcinoma or squamous cell carcinoma are at greater risk of melanoma.
Family History:
Those with a family history of melanoma are at greater risk. If you have a first-degree relative that has had melanoma (such as parent, sibling or child) you're risk increases by 50%.
Heredity plays a major role in melanoma - around one in every 10 patients diagnosed with melanoma has a family member with a history of the disease.
Children in melanoma-prone families need observing carefully as melanoma is likely to appear early in life. often they do not appear until after adolescence, but may arise in much younger children who have a family history of melanoma. It is important therefore for parents to make a point of studying a child's skin frequently from infancy with specialist examinations twice yearly from the age of 10. During adolescence hormonal changes activate moles and special attention should be paid to any changes.
What are normal moles?
Normal moles appear in the first few decades of life in almost everyone and are common small brown spots or growths on the skin. They appear either flat, or elevated and are usually round and regular in shape. Many are caused by sun exposure.
What are abnormal (atypical moles)?
Atypical moles are called Dysplastic Nevi and are unusual benign moles that may resemble melanoma.
It can be difficult to distinguish between dysplastic nevi and early melanomas and sometimes, melanomas will begin within a dysplastic nevus. To establish the difference between such types, a
physician will remove the entire mole or a portion of it for examination in a pathology laboratory.
Some doctors will examine the mole with a dermoscope, which magnifies the mole showing its internal structures and colours that cannot be seen by the naked eye.
Normal Moles - Examples and characteristics:
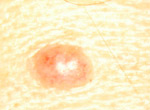



Characteristics of normal moles:
The average young adult has about 10 to 20 such spots or growths.
Generally, normal moles (melanocytic nevi) are:
Shape: symmetrical (one side matches the other in shape), round or oval.
Border: regular edges that are sharp and well-defined.
Colour: uniform in colour throughout - usually tan, brown, or skin colour.
Diameter / size: usually 6 mm (1/4 inch) or smaller.
Uniformity: normal moles usually resemble one another.
Location: more often concentrated on sun-exposed areas of the face, trunk, arms and legs, but can be located anywhere on the body.
Onset: moles usually develop during early childhood and through ages 35-40.
Warning: Having numerous moles, whether normal or atypical, is a risk factor for melanoma.
Pay attention to serious warning signs of melanoma development, such as:
Itching, bleeding, crusting, pain, elevation, swelling, oozing, ulceration, bluish/black colour.
If in any doubt seek immediate medical advice from a skin specialist.
Atypical Moles - Examples and characteristics:




Characteristic of Atypical Moles (Dysplatic Nevi)
Atypical moles are generally large and one of the most important risk factors for melanoma.
These moles can often look like melanomas and are typically:
Shape: often asymmetrical - when one half of the mole does not match the other
Border: irregular and/or with blurred edges, gradually fading into the surrounding skin.
Colour: varies and is irregular with subtle, patches of tan, brown, dark brown, red, blue or black.
Diameter: usually larger than 6 mm (1/4 inch), the size of a pencil eraser, but can be smaller.
Location: most commonly found on the back, chest, abdomen and extremities; but can appear anywhere on the body.
Atypical moles / Dysplastic Nevi and risk of Melanoma:
- People who have atypical moles are at increased risk of developing melanomas.
- The higher number of these moles an individual has, the greater their risk.
- Those who have 10 or more of these moles have 12 times the risk of developing melanoma in comparison to the general population.
- Dysplastic nevi are found significantly more often in melanoma patients than in comparison to the general population.
- Heredity does tend to play a part in their formation.
- People with and family history of dysplastic nevi and melanoma tend to develop melanoma at an earlier age than melanoma patients who donít have dysplastic.
- Those who have dysplastic nevi as well as a family history of melanoma (two or more close blood
relatives with the disease) have an extremely high risk of developing melanoma. - Individuals who have dysplastic nevi, but do not have a family history of melanoma, still face between a 7 to 27 times greater risk of developing melanoma.
- It is reported that approximately 2 to 8 percent of the Caucasian population have these moles.
Some people are severely affected by both normal and atypical moles and are classified as suffering from 'atypical mole syndrome'. They are at exceptional risk of developing melanoma.
People with 'classic' atypical mole syndrome have the following three characteristics:
100 or more moles with 1 or more moles which are atypical.
1 or more moles 8 mm (1/3 inch) or larger in diameter.
Those at greatest risk are individuals with familial atypical multiple mole melanoma syndrome (FAMMM). These individuals not only have atypical mole syndrome, but also have one or more first or second-degree relatives with melanoma.
Warning: ANY mole, growth or pigmented spot that changes in size, shape or colour and/or begins to itch, crust or bleed should be suspected as a melanoma and requires immediate medical attention!
It is also extremely important that individuals with dysplastic nevi take extra caution to practice sun safety measures and never allow themselves to burn.
They should also check their skin at least once a month paying particular attention to moles and have regular professional screening.
The method used to stage melanoma is based mainly on the thickness of the tumour and whether cancer has spread to lymph nodes or other parts of the body.
The staging system is based on the following criteria:
The thickness of the tumour. The thickness is described using the Breslow scale.
Whether the tumour is ulcerated (has broken the skin).
Whether the tumour has spread to the lymph nodes and if the lymph nodes are joined together (matted).
Whether the tumour has spread to other parts of the body.
Early melanomas (Stages 0 and 1) are localised, and more advanced melanomas (Stages 3 and 4) have spread (metastasized) to other parts of the body.
There are also subdivisions within stages.
The following stages are used for melanoma:
Stage 0 melanoma (in situ)
Abnormal melanocytes are in the epidermis (outer layer of the skin).
Stage 1 melanoma.
In stage 1A, the tumour is not more than 1 mm thick, with no ulceration (break in the skin).
In stage 1B, the tumour is either not more than 1 mm thick, with ulceration, OR more than 1 but not more than 2 mm thick, with no ulceration.
Stage 2 melanoma.
In stage 2A, the tumour is either more than 1 but not more than 2 mm thick, with ulceration (break in the skin), OR it is more than 2 but not more than 4 mms thick, with no ulceration.
In stage 2B, the tumour is either more than 2 but not more than 4 mm thick, with ulceration, OR it is more than 4 mm thick, with no ulceration.
In stage 2C, the tumour is more than 4 mm thick, with ulceration.
Stage 3 melanoma.
The tumour may be any thickness, with or without ulceration (a break in the skin), and
(a) cancer has spread to one or more lymph nodes;
(b) lymph nodes with cancer may be joined together (matted);
(c) cancer may be in a lymph vessel between the primary tumour and nearby lymph nodes; and/or
(d) very small tumours may be found on or under the skin, not more than 2 cm away from the primary tumour.
Stage 4 melanoma.
The cancer has spread to other places in the body, such as the lung, liver, brain, bone, soft tissue, or gastrointestinal (GI) tract. Cancer may have spread to places in the skin far away from where it first started.
Survival Rates
Having a thick Melanoma (Breslow thickness >4mm) results in 5-year survival rates of less than 50%.
Having a thin Melanoma (Breslow thickness <1mm) results in 5-year survival rates of more than 95%.
So presenting early with a changing or suspicious mole is vital. Removing a Melanoma whilst it is thin can potentially be curative and life-saving.
Approximate 5-year survival
Melanoma In situ 95-100%
< 1 mm 95-100%
1-2 mm 80-96%
2.1-4 mm 60-75%
>4 mm 50%
People with melanoma will be placed under the care of a multidisciplinary team. This is a team of health professionals including: surgeons and cancer doctors, a specialist nurse, an occupational therapist, and a counsellor or psychologist. This team all work together to plan your care and decide the best way
forward for each patient. Local teams that treat melanoma and other skin cancers are called Local Skin Cancer Multidisciplinary teams (LSMDTs).
Treatment of early stage melanoma (Stages 0-I)
Melanoma is first diagnosed by removing the abnormal mole and a small area of surrounding skin under local anaesthetic. This tissue is then checked thoroughly under a microscope to confirm diagnosis of melanoma.
If it is melanoma, a second operation is performed to remove a larger area of healthy tissue around where the melanoma was. This operation is called a wide local excision.
As long as your doctors are sure that they removed enough tissue, this is all the treatment you need.
The specialist surgeon usually removes between 1cm and 2 cm of tissue from all around the melanoma. However, this is dependant on how thick the melanoma was.
This operation is performed under local anaesthetic, but may require a general anaesthetic if your surgeon is also going to do a test to check the lymph nodes.
This test is called a sentinel lymph node biopsy.
After the treatment
If you had a very early stage melanoma (in situ or stage 0) you will have one appointment at the follow up clinic. Your doctor or nurse will also show you what signs to look out for that would tell you if your melanoma has come back. These include:
- Changes in other moles.
- Dark, mole like, spots appearing near where your melanoma was removed.
- Enlarged glands (lymph nodes) close to where you had the melanoma removed.
If you notice any of these changes, you should contact your specialist or nurse immediately.
If you had a stage 1a melanoma you then have 2 to 4 follow up appointments in the outpatient clinic over the following year. You will also have an appointment to show you which signs to look for that
would indicate recurrence. After that if all is well your doctor may discharge you.
If you had a stage 1b melanoma, you will also have an appointment to show you which signs to look for that would indicate recurrence in addition to appointments in the outpatient clinic every 3 months for 3 years. After that you have appointments every 6 months for another 2 years.
A Specialist Skin Cancer Multidisciplinary team (SSMDTs) which includes specialist surgeons and cancer doctors, a specialist nurse, an occupational therapist, camouflage make up specialist and a counsellor or psychologist, work together to plan your care.
Your first treatment is surgery to remove the melanoma. You then have further surgery called a Wide Local Excision (WLE). This operation removes more tissue to lower the risk of the melanoma coming back in the future.
At the same time as the wide local excision, your doctor may also do a test called a sentinel lymph node biopsy (SLNB). This checks whether the melanoma cells have spread into lymph nodes close to the melanoma and can help determine how likely the melanoma is to come back and if you therefore you need further treatment - however, not all hospitals offer these tests.
Removing the lymph nodes
If the decision is made to remove the lymph nodes a lymph node dissection will be performed which can be a big operation. The type of surgery you have will depend on where your primary melanoma was located in your body. There are large groups of lymph nodes in the neck, armpit and groin and the lymph nodes closest to the primary melanoma would be removed.
Treatment after surgery
Treatment after surgery to prevent it coming back is called adjuvant treatment. According to Cancer Research UK: there is currently no strong research evidence at the moment to show that any adjuvant treatment helps to stop melanoma from coming back or spreading. For this reason, you should only be offered adjuvant treatment within a clinical trial. You may be asked to join a trial if your lymph nodes contained cancer cells.
As well as adjuvant treatment for melanoma in clinical trials, you may have Chemotherapy or Biological therapy. Unfortunately, very little is known about which is the best adjuvant treatment for melanoma.
A type of biological therapy called interferon has been widely used to try to prevent stage 2 or 3 melanoma from coming back. Although it can help to stop melanoma coming back in a small number of people it also causes side effects such as tiredness and depression. The side effects can lower people's quality of life and so doctors don't currently recommend interferon as a standard treatment.
Clinical trials are going on all the time to try to find out the best treatment approach.
You can find details of current trials on the Cancer Research website.
What happens if the melanoma comes back?
Once a stage 2 or 3 melanoma is removed some people are cured and experience no further problems.
However, some people may experience 'locoregional recurrence' which is when the melanoma comes back in the nearby area.
The usual treatment is surgery to remove the new area of melanoma - but if there is more than one area, you may have laser treatment which uses a carbon dioxide laser to destroy the melanoma cells.
If the above treatments do not eradicate the melanoma or if the melanoma deeply penetrates the skin, chemotherapy as capsules or into a vein, radiotherapy, or a new clinical trial may be recommended.
Information from Cancer Research UK indicates that between 15 and 35% of stage 2A melanomas come back after surgery. Between 40 and 70% of stage 2B and 2C melanomas come back and more than half of stage 3 melanomas come back.
Electrochemotherapy
Electrochemotherapy is a treatment used to treat skin cancers, including advanced metastatic melanoma stage lllb/lllc. Electrochemotherapy can be used if surgery is not appropriate or possible.
This treatment works by combining a low dose of a specific chemotherapy drug and applying an electrical pulse directly to the cancer cells. Normally this level of chemotherapy would not be effective against the cancer, but when an electrical pulse is applied directly to the tumour, the cancer cells develop pores which allow the drug to be absorbed. The treatment is specific to the disease area, which means that the whole body does not need to endure the unpleasant effects of chemotherapy. It can also be used to shrink large cancers on the skin, making them easier to remove surgically.
Electrochemotherapy is usually performed under local anesthesia. Your consultant will discuss which is the most suitable treatment for you. It is not available at every hospital but you can be referred to a nearby centre. More information can be found on the NHS choices website or visit www.igeamedical.co.uk.
A Specialist Skin Cancer Multidisciplinary team (SSMDT) including specialist surgeons and cancer doctors, a specialist nurse, an occupational therapist, camouflage make up specialist, and a counsellor or psychologist, work together to plan your treatment and care.
Stage 4 or 'Advanced' melanoma means the cancer has spread from its origin to another part of the body. Cancer that has spread to another part of the body is called secondary cancer or metastases.
The most common place for a Melanoma to spread to is: lungs, liver, bones, brain, abdomen and lymph nodes - however Melanoma can spread to almost anywhere in the body.
The following treatments can be used for advanced melanoma:
Biological Therapy: Drugs used in biological therapy usually aim to boost your immune system to halt or slow growth of cancer cells - some biological treatments target specific enzymes or molecules important to cancer cells.
Chemotherapy: Chemotherapy employs potent drugs that stop or slow the growth of cancer cells by interfering with their ability to divide or reproduce themselves.
Radiotherapy: Radiotherapy uses a focused beam of high energy rays to kill cancer cells. This may be used to shrink melanoma tumours. Sometimes a radioactive source is placed on or in a tumour.
Surgery: Surgery may be used to remove tumours that have spread to other areas of the body.
Clinical trials: Some newer treatments are being tested in clinical trials, your doctor will be able to inform you of these.
Which treatment is right for you will depend on:
- Where your cancer has spread to
- The symptoms you have
- The treatment you have already had
- Changes in the genes within the melanoma tumour
It can be difficult to decide which treatment to try and whether to have treatment at all when you have an advanced cancer. Unfortunately, the treatment will not cure the melanoma but may shrink it or control it for a time.
It is important to think about how the treatment will affect your daily life, whether it may cause side effects, as well as additional stresses such as travelling back and forth to the hospital.
Most importantly, you will need to discuss with your doctor what the treatment you are offered can do to control the melanoma. There may also be a counsellor or specialist nurse at the hospital you could talk to. It can be helpful to talk difficult decisions over with a close relative, friend or even with someone outside your circle of family and friends or someone in the same or similar situation.
Click here for information on organisations that can give you counselling and emotional support >
How serious is my melanoma? This question is often the first that comes to mind when people are told they have a diagnosis of this disease. Many melanomas, especially if caught early, are curable.
However in some cases a diagnosis of advanced or 'metastatic' melanoma (where the cancer has spread) may be given. Advanced melanoma is not curable and its diagnosis has a range of implications.
Advanced melanoma is a serious condition and if you are unclear on any points we encourage you to speak to your doctor to ensure you have all the information you need. Only they will be able to give you the best insight into your particular situation. For everything else, there are always people available and willing to help and some support links are listed below.
The shock of a diagnosis
A diagnosis of advanced melanoma comes as a terrible shock - especially if you have not been experiencing many symptoms. Coming to terms with this potentially life-threatening diagnosis can be a difficult and lengthy process and may leave you feeling apprehensive, fearful, anxious, angry, at times depressed.
Some confront the disease, determined to fight it head-on, whilst others withdraw and don't want to discuss or even think about it - what works for one person may not work for another. However,
developing a coping strategy is important. Although hard, keeping an eye on your emotional well-being and avoiding stress is important. Whilst remaining positive may be easier said than done, there are strategies that can help. Accepting support from friends and family, expressing emotions rather than bottling them up, sharing fears and talking openly about them, and participating fully in decisions about treatment may all help you to feel better and stronger.
Local support services will be available to help you through your disease and organisations such as Macmillan Cancer Support can help put you in touch. There are also a number of online communities where you can meet and talk to other people facing the challenge of advanced melanoma. See the resources section for more information.
Symptoms of advanced melanoma
Advanced melanoma may come with some fairly general symptoms, such as tiredness, loss of appetite and weight loss. Other symptoms will depend on where the melanoma has spread but if you have concerns - and particularly if you have had a melanoma in the past - it's always best to get them checked. If visiting your GP, make sure they understand and appreciate your history with this disease.
If the cancer has spread the symptoms will vary. Secondary tumours in the lungs may cause breathlessness or coughing; in the skeleton, pain or discomfort in your bones; in the brain, headaches, nausea or perhaps weakness in a limb, depending upon which part of the brain has been affected. Your doctor should know from scans where the secondary tumours are and what symptoms they might be expected to cause. It is important to keep a diary of all your symptoms and tell your doctor about them.
Many patients fear pain as a major symptom, however modern pain relief medications are increasingly able to help cope with these. Pain relief should always be available, even in the most advanced disease.
Visiting the doctor and asking questions
In the immediate aftermath of a melanoma diagnosis, questions may tumble over one another. What stage is my melanoma? Can it be cured? Should I ask for a second opinion? What are the treatments? Will it hurt? If it cannot be cured, how long have I got? Understanding and remembering a doctor's answers to these questions can be difficult, especially when you are feeling anxious and upset.
For this reason it is a good idea to write down any questions you have for your doctor, in advance of a consultation. Take a pen and paper with you to write down the answers, or even better, have a friend or partner accompany you to help remember and jot them down. Alternatively, use your smartphone or a digital recorder to record the consultation so you can listen to it later. The doctor should not object to this if asked.
Some questions that you may wish ask if diagnosed with advanced melanoma include:
What Stage is my melanoma at and what does that mean?
What symptoms might I experience?
What treatment will I be given and what are the side effects likely to be?
What are the pros and cons of various treatment options?
What can I expect from treatment, how much better will it make me?
If treatment does not appear to be working, are there clinical trials I can be entered into?
Will I be able to continue working? What should I tell my employer?
What will happen to me? What is the best, and worst case scenario for my future?
Are other people in my family at risk of getting a melanoma?
How do I explain this to my children? What plans do I need to make?
Are there local groups that could help me find more information and support?
Links to organisations that may help you gain further information or emotional support:
For information about treatments used in advanced melanoma visit:
http://www.cancerresearchuk.org/cancer-help/type/melanoma/treatment/advanced-melanoma
http://www.nhs.uk/Conditions/Malignant-melanoma/Pages/Treatment.aspx
Macmillan Cancer Support can help with information on support services available to you:
http://www.macmillan.org.uk
Melanoma glossary can help explain some of the more technical terms you may come across:
http://www.melanoma.org/learn-more/glossary-melanoma-terms
or: http://www.melanomainternational.org/melanoma_info/glossary.html
Prevention is better than cure.
Whilst most skin cancers and precancers are curable if detected early, prevention is always better than cure. 80-90% of all skin cancers can be avoided by ensuring that appropriate precautions are
taken during time spent in the sun.
Always follow the five S's of sun safety below and make sure you stick to these golden rules:
- Avoid tanning and never allow your skin to burn
- Never use indoor tanning devices
- Examin your skin thoroughly at least once a month
- If you are worried or uncertain about any abnormality, seek immediate professional advice
For those that have suffered from a precancer, or skin cancer, particular care and attention to covering up and shading from the sun is very important as well as thoroughly checking your skin more frequently for signs of recurrence or developments of new abnormalities.
The Five S's of Sun Safety:

SLIP on a T-shirt
Always keep shoulders covered
as they can easily burn in the sun

SLOP on good quality sunscreen
Always use a sunscreen with a minimum SPF of 30 with broad spectrum UVA protection
Apply generously 20 mins before going outside and reapply at least every 2 hours

SLAP on a broad brimmed hat
Wear a legionnaire or broad-brimmed hat to help shade the face, neck and ears
which can easily burn in the sun.

SLIDE on quality sunglasses
Wear quality (preferrably wrap-around) sunglasses to help protect
your eyes that can be damaged by the sun.

SHADE - Seek shade whenever possible
Always seek shade, particularly between 11am and 3pm when the sun's
UV penetration is strongest.
THE EARLY DETECTION OF SKIN CANCER CAN REDUCE YOUR RISK OF POTENTIAL DISFIGURMENT OR EVEN DEATH.
Make sure you check your skin thoroughly at least once a month for signs of change.
Remember what to look out for when checking your skin - download and print off our early detection fact sheet.
DOWNLOAD NOWREMEMBER: If you are worried or uncertain about any suspicious patch, lump, mole or lesion - go to your GP and seek professional advice from a skin specialist or dematologist immediately.
REMEMBER: PREVENTION IS BETTER THAN CURE!
Always use the
Five S's of Sun
Safety & never allow
your skin to burn!







